Is Vitamin D linked to diabetes?
- Home
- Natural Remedies
- Diabetes Vitamin D Deficiency & Benefits
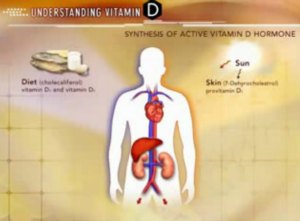
Vitamin D deficiency may contribute to insulin resistance and inflammation, potentially increasing the risk of diabetes, emphasizing the importance of monitoring and maintaining adequate vitamin D levels.
Is there a link between vitamin D deficiency and diabetes?
Yes, there is evidence suggesting a link between vitamin D deficiency and diabetes.
Several studies have indicated that low levels of vitamin D may be associated with an increased risk of developing type 2 diabetes, as well as complications in individuals already diagnosed with diabetes.
1. Insulin Sensitivity: Vitamin D is thought to play a role in improving insulin sensitivity, which is crucial for the regulation of blood sugar levels.
Insulin resistance, where the body's cells do not respond effectively to insulin, is a key feature of type 2 diabetes. Low levels of vitamin D may exacerbate insulin resistance, potentially contributing to the development of diabetes.
2. Inflammation: Vitamin D has anti-inflammatory properties, and inflammation is believed to be involved in the development of type 2 diabetes.
Vitamin D deficiency may contribute to increased inflammation, which could further impair insulin sensitivity and glucose metabolism.
3. Pancreatic Function: Vitamin D receptors are present in pancreatic beta cells, which are responsible for producing insulin.
Vitamin D may play a role in preserving beta cell function and promoting insulin secretion. Deficiency in vitamin D could potentially compromise pancreatic function, leading to difficulties in blood sugar regulation.
4. Obesity: Obesity is a significant risk factor for type 2 diabetes, and individuals with obesity are more likely to have lower levels of vitamin D.
It's unclear whether low vitamin D levels contribute to obesity or if obesity leads to lower vitamin D levels due to reduced sunlight exposure (as vitamin D can be synthesized in the skin with sunlight exposure) or altered metabolism.
Nonetheless, the association between obesity, vitamin D deficiency, and diabetes risk is an area of active research.
What are the symptoms of vitamin D deficiency in people with diabetes?
In people with diabetes specifically, vitamin D deficiency may exacerbate symptoms related to diabetes complications, such as neuropathy or cardiovascular issues.
However, it's essential to note that these symptoms can also be attributed to diabetes itself or other underlying health conditions.
Therefore, diagnosing vitamin D deficiency in people with diabetes typically involves blood tests to measure serum vitamin D levels.
Following are some symptoms related to vitamin D deficiency in diabetics:
- Fatigue: Feeling tired or fatigued even after adequate rest.
- Muscle Weakness: Weakness in muscles, which may affect mobility and physical performance.
- Bone Pain: Pain or tenderness in the bones, often in the lower back, hips, or legs.
- Bone Fractures: Increased risk of fractures or decreased bone mineral density due to weakened bones.
- Depression: Mood changes, including feelings of depression or low mood.
- Impaired Wound Healing: Slower healing of wounds or injuries.
- Frequent Illness: Increased susceptibility to infections due to weakened immune function.
- Hair Loss: Experiencing hair loss or thinning hair.
- Poor Dental Health: Increased risk of dental problems such as gum disease or tooth decay.
- Impaired Cognitive Function: Some studies suggest a potential link between vitamin D deficiency and cognitive impairment.
Should people with diabetes get their vitamin D levels tested regularly?
While there isn't a universal recommendation for routine vitamin D testing in people with diabetes, it may be prudent for individuals with diabetes to discuss vitamin D testing with their healthcare provider, especially if they have risk factors for vitamin D deficiency or are experiencing symptoms suggestive of deficiency.
Factors that may increase the risk of vitamin D deficiency in people with diabetes include:
a. Limited Sun Exposure: Individuals who have limited sun exposure, either due to geographic location, lifestyle factors, or spending most of their time indoors, may be at increased risk of vitamin D deficiency.
b. Obesity: Obesity is a risk factor for both type 2 diabetes and vitamin D deficiency. Adipose tissue can sequester vitamin D, making it less available for use by the body.
c. Malabsorption Issues: Some individuals with diabetes may have gastrointestinal conditions or procedures that affect the absorption of nutrients, including vitamin D.
d. Certain Medications: Some medications commonly used to manage diabetes, such as certain anticonvulsants or glucocorticoids, can interfere with vitamin D metabolism.
e. Older Age: Older adults with diabetes may have a higher risk of both vitamin D deficiency and diabetes-related complications.
f. Ethnicity: People with darker skin pigmentation may have lower vitamin D levels because melanin reduces the skin's ability to produce vitamin D in response to sunlight exposure.
What does the research say about the relationship between vitamin D and diabetes?
Overall, while the evidence supporting a relationship between vitamin D and diabetes is compelling, further research is needed to elucidate the underlying mechanisms and determine the potential benefits of vitamin D supplementation in diabetes prevention and management.
Individualized approaches considering factors such as baseline vitamin D status, genetics, lifestyle factors, and comorbidities are essential for optimizing diabetes care.
Research on the relationship between vitamin D and diabetes suggests several key findings:
1. Vitamin D Deficiency and Diabetes Risk: Numerous observational studies have found associations between low vitamin D levels and an increased risk of developing type 2 diabetes.
These studies have often controlled for confounding factors such as age, obesity, and physical activity. While correlation does not imply causation, these findings suggest that vitamin D deficiency may be a risk factor for diabetes development.
2. Insulin Sensitivity and Beta Cell Function: Vitamin D may play a role in improving insulin sensitivity and preserving pancreatic beta cell function, which are essential for maintaining normal blood sugar levels.
Some research indicates that vitamin D supplementation may improve insulin sensitivity and reduce the risk of insulin resistance, a hallmark of type 2 diabetes.
3. Inflammatory Pathways: Vitamin D has anti-inflammatory properties, and inflammation is believed to contribute to the development of type 2 diabetes.
Low vitamin D levels may exacerbate inflammation, potentially worsening insulin resistance and glucose metabolism.
4. Genetic Factors: Genetic studies have identified gene variants associated with both vitamin D metabolism and diabetes risk.
Variations in genes involved in vitamin D synthesis or receptor function may influence an individual's susceptibility to both vitamin D deficiency and diabetes.
5. Clinical Trials: Intervention studies investigating the effects of vitamin D supplementation on diabetes outcomes have yielded mixed results.
While some trials have shown improvements in insulin sensitivity, glycemic control, and diabetes risk factors with vitamin D supplementation, others have found no significant effects.
The heterogeneity of study designs, populations, dosages, and follow-up periods may contribute to these discrepancies.
6. Complications Management: Vitamin D deficiency may exacerbate complications associated with diabetes, such as cardiovascular disease, neuropathy, and impaired wound healing.
Optimizing vitamin D status through supplementation or other means may help mitigate these risks and improve overall health outcomes in individuals with diabetes.
Can vitamin D deficiency increase the risk of complications in diabetes?
There is evidence to suggest that vitamin D deficiency may increase the risk of complications in diabetes.
Several studies have shown associations between low levels of vitamin D and various complications of diabetes, including cardiovascular disease, neuropathy, nephropathy, and retinopathy.
Vitamin D is known to play a role in regulating insulin secretion and sensitivity, as well as in reducing inflammation and improving endothelial function.
Therefore, deficiency in vitamin D may exacerbate insulin resistance and inflammation, which are key factors in the development and progression of diabetes complications.
However, it's important to note that while there is evidence of an association between vitamin D deficiency and diabetes complications, more research is needed to fully understand the mechanisms involved and the potential benefits of vitamin D supplementation in preventing or managing these complications.
Additionally, other factors such as genetics, lifestyle, and comorbidities may also influence the relationship between vitamin D deficiency and diabetes complications.
Therefore, it is a must to consult with your healthcare provider for personalized advice on vitamin D supplementation and management of current condition.
Does vitamin D supplementation help manage diabetes?
The role of vitamin D supplementation in managing diabetes is still an area of active research, and findings have been mixed.
Some studies suggest that vitamin D supplementation may have beneficial effects on certain aspects of diabetes management, while others have found no significant effects.
Several potential mechanisms have been proposed for how vitamin D may affect diabetes:
1. Insulin Sensitivity: Vitamin D may improve insulin sensitivity, which is beneficial for people with diabetes, particularly those with insulin resistance.
2. Beta-Cell Function: Vitamin D may help preserve beta-cell function, which is responsible for producing insulin in the pancreas.
3. Inflammation: Vitamin D has anti-inflammatory properties, and reducing inflammation may improve insulin sensitivity and glucose metabolism.
4. Blood Pressure Regulation: Vitamin D may help regulate blood pressure, which is important for managing diabetes and reducing the risk of cardiovascular complications.
However, the evidence regarding the effectiveness of vitamin D supplementation in diabetes management is not conclusive.
Some studies have shown improvements in measures such as insulin sensitivity and glycemic control with vitamin D supplementation, while others have found no significant effects.
It's important to note that the effectiveness of vitamin D supplementation may vary depending on factors such as baseline vitamin D levels, individual differences in response to supplementation, and other factors such as diet, lifestyle, and genetics.
Therefore, while vitamin D supplementation may be considered as part of a comprehensive approach to managing diabetes, it should not replace other established treatments such as medication, diet, exercise, and regular monitoring of blood glucose levels.
How much vitamin D should people with diabetes take?
The recommended daily intake of vitamin D can vary depending on factors such as age, sex, health status, and individual needs.
For people with diabetes, there isn't a specific recommended dosage of vitamin D that applies universally.
Instead, recommendations should be tailored based on individual factors and the guidance of a healthcare provider.
The Institute of Medicine (IOM) provides general recommendations for vitamin D intake, suggesting that most adults need about 600-800 IU (International Units) of vitamin D per day to maintain adequate blood levels.
However, some research suggests that higher doses may be needed for certain populations or health conditions.
For individuals with diabetes, especially those who are deficient in vitamin D or have difficulty absorbing it, higher doses of vitamin D supplementation may be recommended.
However, it's essential to consult with a healthcare provider to determine the appropriate dosage based on factors such as:
- Blood levels of vitamin D: A blood test can measure the concentration of 25-hydroxyvitamin D [25(OH)D], which is used to assess vitamin D status. Based on the results, a healthcare provider can recommend appropriate supplementation.
- Individual health status: People with certain medical conditions or risk factors may require higher doses of vitamin D. For example, individuals with diabetes and concurrent conditions such as obesity or malabsorption disorders may need higher doses to achieve adequate blood levels.
- Sun exposure: Vitamin D can also be synthesized in the skin upon exposure to sunlight. Factors such as geographic location, time of year, skin pigmentation, and sunscreen use can affect the body's ability to produce vitamin D from sunlight.
- Other medications and supplements: Some medications and supplements can interact with vitamin D or affect its absorption and metabolism. It's essential to consider potential interactions when determining the appropriate dosage.
Overall, the dosage of vitamin D supplementation for people with diabetes should be individualized based on their specific needs and circumstances. Regular monitoring of vitamin D levels and ongoing evaluation by the caring doctor/nurse can help ensure that supplementation is safe and effective.
Are there any natural ways to increase vitamin D levels for people with diabetes?
Yes, there are several natural ways to increase vitamin D levels for people with diabetes, as well as for the general population.
These methods include:
1. Sunlight exposure: The most natural way to increase vitamin D levels is through exposure to sunlight.
When your skin is exposed to sunlight, it produces vitamin D. Aim for about 10-30 minutes of sun exposure on your arms, legs, back, or face without sunscreen several times a week.
The amount of sun exposure needed varies depending on factors such as skin type, time of day, season, and geographic location.
2. Dietary sources: While there are limited food sources of vitamin D, including fatty fish (such as salmon, mackerel, and tuna), egg yolks, cheese, and fortified foods (such as fortified milk, orange juice, and cereals), these may not provide sufficient amounts for many people to reach optimal vitamin D levels.
However, incorporating these foods into your diet can still contribute to your overall vitamin D intake.
3. Supplementation: If natural sources are insufficient or impractical, vitamin D supplements are available over-the-counter. It's essential to consult with your caring doctor/nurse before starting any supplementation regimen to determine the appropriate dosage based on your individual needs and circumstances.
4. Maintaining a healthy weight: Obesity has been associated with lower vitamin D levels.
By achieving and maintaining a healthy weight through a balanced diet and regular physical activity, you may be able to improve your vitamin D status.
5. Limiting sunscreen use: While sunscreen is crucial for protecting against skin cancer and sunburn, it can also block the production of vitamin D in the skin.
If you're planning to be in the sun for an extended period, consider applying sunscreen after the initial exposure period or on areas of the body not exposed to the sun.
It's important to note that while these natural methods can help increase vitamin D levels, they may not be sufficient for everyone, especially those with certain medical conditions, limited sun exposure, or other factors affecting vitamin D absorption and metabolism.
Therefore, regular monitoring of vitamin D levels and consultation with a healthcare provider are essential for managing vitamin D status effectively.
|
Written by Dr.Albana Greca Sejdini, Md, MMedSc Medically reviewed by Dr.Ruden Cakoni, MD, Endocrinologist |
Last reviewed 02/20/2024 |
References:
References:
- Vitamin D deficiency and Diabetic Retinopathy
- Supplements with vitamin D and Insulin Resistance
- Role of Vitamin D in Diabetes, Metabolic Syndrome and Insulin Resistance
- Does vitamin D have a role in Diabetes?
- Beta Cell Dysfunction and Insulin Resistance
- Relationship between Vitamin D and Insulin Resistance
- Genetic Susceptibility and the Response to Supplementation
- Effects of Vitamin D Supplementation on Metabolic and Oxidative Stress Markers in Diabetics
- Vitamin D and Diabetic Complications
- Vitamin D deficiency and Chronic Liver Disease
Explore more vitamins And Minerals.
Diabetes complications Questions or Problems? Get Help Here
This is the place where you can ask a question about any aspect of diabetes complications.
It's free and it's easy to do. Just fill in the form below, then click on "Submit Your Question".