Diabetes Leg Pain Relief
- Home
- Complications
- Diabetes Leg Pain Relief
< Previous 3 | 8 NEXT >
Diabetic leg pain is a common and often disabling consequence that can be caused by peripheral neuropathy and peripheral artery disease (PAD). Not only does this discomfort make daily activities more difficult, but it also raises the likelihood of developing infections and ulcers.
In order to avoid additional issues and keep people with diabetes generally healthy, it is essential to understand the reasons for and ways to treat diabetic leg pain.
What causes leg pain in diabetes?
Numerous factors, primarily diabetes-related complications, contribute to leg pain in people with the disease.
Here are the main causes:
- Peripheral Neuropathy due to Nerve Damage: High blood sugar levels can damage the nerves, particularly in the legs and feet, leading to a condition known as diabetic peripheral neuropathy. Tingling, burning, numbness, and pain are symptoms that arise from this injury.
- Peripheral Artery Disease (PAD) Due to Poor Circulation: Diabetes can narrow and harden blood vessels, reducing blood flow to the lower extremities and increasing the risk of peripheral artery disease (PAD). Peripheral artery disease (PAD) manifests most visibly during claudication, or very strenuous physical exertion, and causes pain, cramping, and discomfort.
- Diabetic Amyotrophy due to Muscle Weakness: An uncommon consequence of diabetes is diabetic amyotrophy, which manifests as a loss of muscle mass and strength in the legs, hips, buttocks, or thighs as a result of damage to the nerves that supply these areas. A different name for it is proximal neuropathy.
- Infections and ulcers due to wounds and sores: Diabetics are at increased risk for wound infections and ulcers, particularly in the foot, because of decreased blood flow and nerve loss. Untreated, these can worsen to a point where they cause excruciating pain. If things go horribly wrong, amputation may be necessary.
- Charcot Joint due to Joint Damage: Rarely, diabetes can develop a condition known as Charcot joint, which manifests as a weakening and eventual fracture of the foot's bones, accompanied by pain, swelling, and deformities.
- Inflammation characterized by swelling and pain: Chronic inflammation due to diabetes can cause pain and discomfort in the legs as tissues become inflamed and swollen.
Managing blood sugar levels, maintaining a healthy lifestyle, and regular check-ups with your caring doctor are essential to preventing and managing these complications.
How can I tell if my leg pain is related to diabetes?
Determining if your leg pain is related to diabetes involves looking for specific symptoms and considering your medical history.
Following, I'll try to explain some indicators:
Type of Pain: Diabetes-related leg pain often manifests as burning, tingling, numbness, or sharp, stabbing pain. This is commonly due to peripheral neuropathy.
Timing and Activity: Pain that worsens at night or with prolonged activity could be linked to diabetic nerve damage or peripheral artery disease (PAD).
Other symptoms include:
Numbness or Loss of Sensation: A reduced ability to feel temperature changes or pain in the legs and feet.
Muscle Weakness: Difficulty in movement or muscle weakness in the legs.
Skin Changes: dry, cracked skin, changes in color, or the presence of ulcers or sores that heal slowly.
Circulation Issues: Symptoms like cramping during physical activity (claudication) may indicate PAD, a common diabetes complication.
Medical History: A known diagnosis of diabetes, particularly if blood sugar levels have been poorly controlled, increases the likelihood that leg pain is related to the condition.
There are some physical exams and tests that are run if any of the above-mentioned symptoms are noted, including:
Monofilament Test: Your caring doctor uses a monofilament tool to check for loss of sensation.
Ankle-Brachial Index (ABI): measures blood flow and helps diagnose PAD.
Nerve Conduction Studies: Assess the function of the peripheral nerves.
When should I see a doctor for diabetes leg pain?
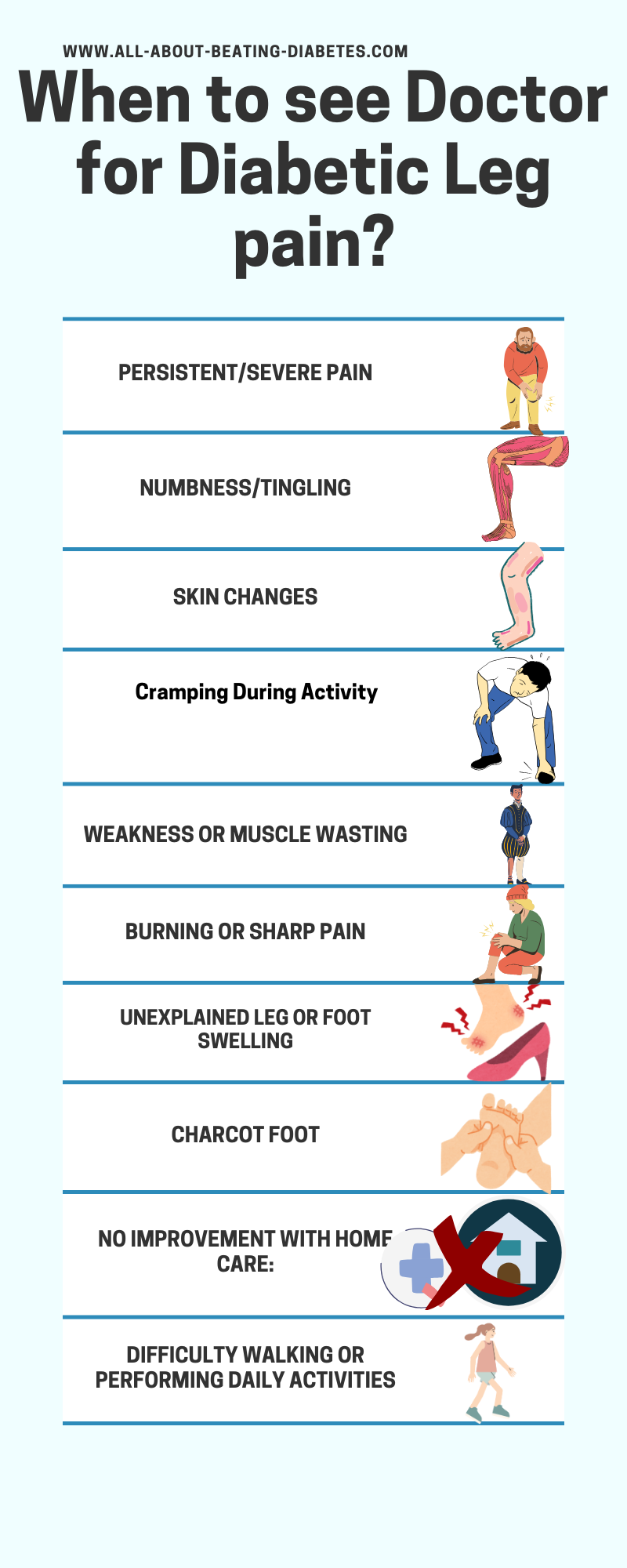
Early intervention can prevent complications and improve your quality of life.
Always communicate with your caring doctor about any new or worsening symptoms related to diabetes.
This is particularly true if you are also experiencing one or all of the worsening symptoms of diabetes leg pain.
Worsening in muscle weakness, persistent pain, feeling numbness or tingling, sharp pain, Charcot foot, or unexplained leg or food swelling, serve as a ringing bell to see your caring doctor as soon as possible.
Apart from endocrinologists, neurologists and podiatrists are highly recommended to consult further.
Are there specific home remedies that can help with diabetes leg pain?
The very first piece of advice we give our patients is to start with some beneficial home remedies to ease leg pain. I know that sometimes any of you might find it difficult, but persistence makes a difference.
Some of the home remedies and lifestyle changes that can help manage diabetes leg pain include:

Warm Bath:
Soaking your legs in warm water can help soothe pain and improve circulation. Avoid water that's too hot to prevent burns.

Massage:
Gently massaging your legs can alleviate pain and improve blood flow.
You can use over-the-counter creams or oils designed for pain relief.
Or you can make an appointment with a physiotherapist to start more specific massage therapy according to your actual health problems and body needs.

Elevating Legs:
Elevate your legs when sitting or lying down to reduce swelling and improve circulation.

Cold and Heat Therapy:
Alternating between cold and heat pads can reduce inflammation and pain.
Use cold packs for 15–20 minutes, then switch to heat pads.

Essential Oils:
Applying essential oils like lavender or peppermint mixed with a carrier oil can provide relief through their soothing properties.
Furthermore, rosemary oil carries antiseptic properties and can help reduce skin inflammation and infection.
What lifestyle changes will help care diabetes leg pain?
Lifestyle changes are also very important in reducing leg pain. Remember to be consistent in order to succeed. Even small or underestimated things matter a lot in managing the pain.
The most effective lifestyle changes include the following:
Blood Sugar Control:
Maintaining stable blood sugar levels is crucial.
Follow your doctor's recommendations on diet, medication, and close monitoring.

Healthy Diet:
Focus on a balanced diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats.
Avoid processed foods, sugary drinks, and foods high in saturated and trans fats.
Weight Management:
If you are overweight, losing even a small amount of weight can significantly reduce your pain and improve your overall health.

Quit Smoking:
Smoking impairs blood flow and can worsen diabetes complications.
Seek medical support to quit smoking if you cannot succeed alone.
Can exercise help reduce leg pain in diabetics?
Yes, exercise can help reduce leg pain in diabetics by improving blood circulation, reducing inflammation, strengthening muscles, and maintaining overall health.
Here’s how exercise can benefit individuals with diabetes-related leg pain:
Improves blood circulation:
Regular physical activity enhances blood flow, which can alleviate pain and prevent complications associated with poor circulation, such as peripheral artery disease (PAD).
Reduces Inflammation:
Exercise has anti-inflammatory effects that can help reduce pain and swelling in the legs.
Strengthens Muscles:
Building muscle strength helps support the joints and reduce the strain on the legs, leading to less pain.
Enhances Nerve Health:
Physical activity can help manage blood sugar levels and improve nerve function, potentially reducing the symptoms of diabetic neuropathy.
Helps with Weight Management:
Maintaining a healthy weight through exercise reduces the load on the legs and feet, decreasing pain and the risk of complications.
Improves Flexibility and Balance:
Stretching and balance exercises can help prevent falls and injuries, which are critical for individuals with diabetes.
Recommended Types of Exercise
 |
Aerobic Exercise: Activities such as walking, swimming, cycling, and dancing improve cardiovascular health and circulation. Aim for at least 30 minutes most days of the week. |
 |
Strength Training: Use resistance bands, weights, or bodyweight exercises like squats and lunges to build muscle strength. Aim for two to three sessions per week. |
 |
Flexibility Exercises: Stretching exercises, yoga, and Pilates improve flexibility, reduce stiffness, and enhance overall mobility. |
 |
Balance Exercises: Activities like tai chi or specific balance exercises can help prevent falls and improve stability. |
Tips for Exercising with Diabetes-Related Leg Pain
Start Slowly:
Begin with low-impact exercises and gradually increase intensity and duration to avoid overexertion.
Warm Up and Cool Down:
Always warm up before exercising and cool down afterward to prevent injuries and improve muscle recovery.
Wear proper footwear.
Use well-fitted, supportive shoes to protect your feet and reduce pain during exercise.
Monitor blood sugar levels:
Check your blood sugar before, during, and after exercise to ensure it stays within a safe range. Keep snacks or glucose tablets handy in case of low blood sugar.
Stay Hydrated:
Drink plenty of water before, during, and after exercise to stay hydrated.
Listen to your body:
Pay attention to how your body feels during exercise. If you experience severe pain, dizziness, or shortness of breath, stop exercising and consult a healthcare professional.
Consult a healthcare provider.
Before starting a new exercise regimen, especially if you have any complications or other health conditions, consult with your healthcare provider for personalized advice.
How can I prevent leg pain if I have diabetes?
Preventing leg pain if you have diabetes involves a combination of managing your diabetes effectively and adopting lifestyle changes to support overall leg and foot health.
Here are some key strategies:
1. Maintain Blood Sugar Control
Monitor Blood Glucose: Follow your doctor's advice and regularly check your blood sugar levels.
Medications: Take prescribed diabetes medications or insulin as directed.
Healthy Diet: Follow a balanced diet that helps keep your blood sugar levels stable. Focus on whole grains, fruits, vegetables, lean proteins, and healthy fats. Avoid sugary drinks and processed foods.
2. Regular Exercise
Aerobic Exercise: Engage in at least 30 minutes of moderate-intensity aerobic activity, such as walking, swimming, or cycling, most days of the week.
Strength Training: Include resistance exercises to build muscle strength.
Flexibility Exercises: Stretch regularly to maintain flexibility and prevent stiffness.
3. Proper Foot Care
Daily Inspections: Check your feet daily for any cuts, blisters, redness, swelling, or changes in color.
Hygiene: Wash your feet daily with lukewarm water and mild soap. Dry them thoroughly, especially between the toes.
Moisturize: Apply moisturizer to prevent dry skin, but avoid the areas between your toes to prevent fungal infections.
Nail Care: Trim your toenails straight across and file the edges to prevent ingrown nails.
4. Wear Proper Footwear
Supportive Shoes: Choose well-fitting shoes that provide good support and cushioning. Avoid tight or poorly fitting shoes.
Socks: Wear moisture-wicking socks to keep your feet dry and reduce the risk of blisters.
5. Quit Smoking
Smoking reduces blood flow and can worsen diabetes complications. Seek help to quit smoking if necessary.
6. Weight Management
Maintaining a healthy weight reduces pressure on your legs and improves overall health. Even a small amount of weight loss can make a difference.
7. Stay Hydrated
Drink plenty of water to stay hydrated and support overall health.
8. Stress Management
Practice stress-reducing techniques such as meditation, deep breathing, yoga, or hobbies that you enjoy.
9. Avoid Alcohol and Limit Caffeine
Reduce alcohol intake and limit caffeine, as these can affect blood sugar levels and overall health.
10. Regular Medical Check-ups
Visit your healthcare provider regularly for check-ups. Ensure your feet are examined at each visit.
Peripheral Neuropathy Screening: Regular screening for nerve damage can help catch issues early.
11. Preventive Care
Vaccinations: Stay up-to-date with vaccinations to prevent infections that could complicate diabetes management.
Blood Pressure and Cholesterol Control: Manage these conditions as they can affect circulation and increase the risk of leg pain.
What are the best footwear options for managing diabetes-related leg pain?
Choosing the right footwear is crucial for managing diabetes-related leg pain and preventing complications.
Here are the best footwear options and considerations:
Best Footwear Options

Diabetic Shoes:
- Specifically designed for individuals with diabetes.
- Provide extra depth and width to accommodate foot deformities and orthotics.
- Feature seamless interiors to prevent friction and blisters.
- Offer additional cushioning and support.
 |
Orthopedic Shoes:
|
 |
Athletic Shoes:
|
 |
Custom Orthotics:
|
 |
Sandals with arch support:
|
 |
Boots with support:
|
Key features to look for when choosing diabetic footwear
Proper Fit:
Shoes should be snug but not tight. There should be about half an inch of space between the toes and the end of the shoe.
Avoid shoes that are too loose, as they can cause friction and blisters.
Wide Toe Box:
It provides ample room for the toes to move and prevents cramping and pressure points.
Seamless Interior:
Reduces the risk of friction, blisters, and sores.
Good arch support:
It helps distribute weight evenly and reduces strain on the feet and legs.
Cushioning:
Provides comfort and absorbs shock to reduce impact on the feet and legs.
Breathable Material:
It keeps feet dry and reduces the risk of fungal infections.
Adjustable Closures:
Velcro straps, laces, or buckles allow for a customized fit and better support.
Tips for Choosing the Right Footwear
Shop Later in the Day:
Feet tend to swell throughout the day, so shopping in the afternoon or evening ensures a better fit.
Bring Your Orthotics:
If you use custom orthotics, bring them with you to ensure the shoes fit properly with the inserts.
Check for Sufficient Depth:
Ensure there is enough depth in the shoes to accommodate any foot deformities or swelling.
Consult a Podiatrist:
A podiatrist can provide personalized recommendations and custom orthotics if needed.
|
Written by Dr.Albana Greca Sejdini, Md, MMedSc Medically reviewed by Dr.Ruden Cakoni, MD, Endocrinologist |
Last reviewed: 7.26.2024 |
Related videos:
Diabetes complications Questions or Problems? Get Help Here
This is the place where you can ask a question about any aspect of diabetes complications.
It's free and it's easy to do. Just fill in the form below, then click on "Submit Your Question".