- Home
- blood sugar levels
- acceptable glucose level
What Is Acceptable Blood Glucose Level For Diabetics?
It is important to diabetics to find out what their acceptable levels should be
Knowing your own “acceptable” blood glucose levels is one of the most important parts of living safely and confidently with diabetes. These targets act like a personal map: they show you which numbers are safe, which are a warning, and when you need to take action or call your doctor.
If your blood sugar regularly goes too high, over time it can damage blood vessels and nerves. This increases the risk of heart attack, stroke, kidney disease, eye problems, and nerve pain as main complications.
On the other hand, if your blood sugar drops too low (hypoglycemia), you can feel shaky, sweaty, confused, or even lose consciousness. Clear personal targets help you avoid both extremes.
When you know your acceptable fasting, pre-meal, and after-meal ranges, every reading becomes useful information—not just a scary number. You can see how food, physical activity, stress, illness, and medication affect you, and then adjust your habits accordingly.
Most importantly, acceptable levels are individual. Age, other illnesses, pregnancy, and risk of hypoglycemia all matter. That’s why as a diabetic, you should discuss and confirm your own targets with your caring doctors, then use those numbers to guide everyday decisions and long-term control of diabetes.
What are acceptable blood glucose levels?
"Acceptable" blood glucose levels usually mean ranges that are considered safe and healthy for most people. They vary depending on the context and individual circumstances.
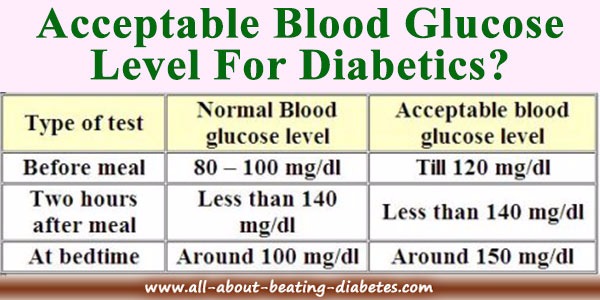
Generally, for someone without diabetes, a normal fasting blood glucose level is typically between 70 and 100 milligrams per deciliter (mg/dL) or 3.9–5.5 mmol/L. Fasting means after 8 or more hours without food, like in the morning for example.
Two hours after eating, it is generally acceptable if it stays below 140 mg/dL or 7.8 mmol/L.
For individuals with diabetes, target blood glucose levels are a bit higher and can differ based on their specific treatment plan and goals. However, they are between the normal and ideal sugar level.
A common goal for many adults is 80–130 mg/dL (4.4–7.2 mmol/L) before meals, and under 180 mg/dL (10 mmol/L) about 1–2 hours after starting a meal, and around 150 mg/dl at bedtime. Some people (for example, older adults, those with heart disease, or those at high risk of low blood sugar) may have slightly higher “acceptable” targets to stay safe.
Any value below 70 mg/dL is usually considered too low (hypoglycemia) and needs quick treatment.
Repeated readings above 180–200 mg/dL, especially after meals, suggest blood sugar is often too high, and the treatment plan may need adjustment. Always confirm your own target range with your caring doctor.
As you may see, these are high but not worrying figures for a diabetic. Although the ideal sugar level is under 100mg/dl; however, you cannot achieve this. Therefore, there exist a "tolerance level" for diabetics.
Even though there is some tolerance in “acceptable” ranges, you should still aim to keep your blood glucose as close to normal as safely possible. You may not achieve this right away, but over time it should become one of your main goals in diabetes management.
Don’t become comfortable with persistent readings over 120 mg/dL just because they are considered acceptable. The closer you keep your blood glucose to your personal target range, the better you protect yourself from long-term diabetes complications.
A practical step is to create your own blood glucose log. Write down every reading with the date, time, and notes about food, activity, or medication. This will help you and your healthcare team see patterns and evaluate how well you’re managing your diabetes.
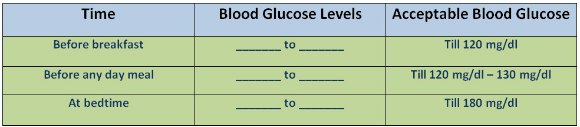
The sample blood sugar table below can serve as a model for designing your own log and a simple chart to visualize your progress.
By keeping a regular blood glucose log, you turn your numbers into a powerful tool instead of something to fear. Note the date, time, blood sugar result, what you ate, your medication/insulin dose, and any exercise or stress. Over days and weeks, patterns begin to appear: you may notice certain foods spike your levels, or that a short walk after dinner keeps your readings steadier. These insights help you and your healthcare team fine-tune your treatment plan and move toward more stable, healthy blood glucose levels.
Managing diabetes is demanding. It often means saying “no” to cravings, planning your meals, and being more active even when you’re tired. It also means slowly letting go of old habits—frequent snacking, oversized portions, sugary drinks—that can quietly worsen your control. This is not about perfection; it’s about progress.
When the journey feels difficult, remind yourself that you are the central decision-maker in your diabetes care. You hold the power to make small, steady changes: adding an extra 10 minutes of walking, replacing one sugary drink per day with water, or checking your blood sugar one more time each week. These may seem minor, but over time they add up to better control and fewer complications.
You don’t have to carry this alone. Your healthcare team (doctor, nurse, dietitian, diabetes educator) can help you set realistic targets, adjust medications, and interpret your log. Support groups, online communities, and family members can offer encouragement, share practical tips, and remind you that setbacks are normal.
Think of each day as a new chance, not a test you already failed. By taking charge, using your blood glucose log, and making deliberate, gradual changes, you can greatly improve your blood sugar control and protect your long-term health. You are not alone in this—and every small, consistent step you take is a real victory against diabetes.
Related topics:
- Find out what the Normal Blood Glucose Level is.
- Get to know the Fasting Blood Glucose Level and what to do in case of high figures.
- Understand the numbers and limits related to Average Blood Glucose Level.
- How to read and interpret the results of a Blood Glucose Tolerance Test?
|
Written by Dr.Albana Greca Sejdini, Md, MMedSc Medically reviewed by Dr.Ruden Cakoni, MD, Endocrinologist |
Last reviewed 11/25/2025 |
References:
- Checking blood sugar for diabetics-ADA
- Chart for Adults with diabetes
- Standards for diabetes Care
- IDF Clinical Practice Recommendations for Primary Care
Diabetes complications Questions or Problems? Get Help Here
This is the place where you can ask a question about any aspect of diabetes complications.
It's free and it's easy to do. Just fill in the form below, then click on "Submit Your Question".
What Other Visitors Have Asked
Click below to see contributions from other visitors to this page...
BLOOD SUGAR READINGS Not rated yet
QUESTION : Hi,
My machine reads 7.5. How do you read in other ways like say 120, what is the equivalence?
ANSWER : Hi Jennifer,
I understand …