- Home
- Your Diabetic Information Center
- Glycemic index of foods – the info you must have
Glycemic Index Foods for Diabetes Blood Sugar Control
A Doctor’s Explanation for Everyday Eating Decisions
Why People With Diabetes Care About GI
Blood sugar control is not only about how many carbohydrates are eaten but also about how quickly they are absorbed.
Foods with a high glycemic index are digested rapidly and can cause:
- Sudden blood glucose spikes
- Increased insulin demand
- Post-meal fatigue or hunger
Low glycemic index foods are digested more slowly and often:
- Produce gentler rises in blood sugar
- Improve post-meal glucose stability
- Support appetite control
- Help reduce glucose variability throughout the day
From a medical perspective, choosing lower GI foods more often may support better long-term metabolic control when combined with appropriate portions, regular monitoring, and an overall balanced diet.
What's the Glycemic Index?
Many people living with diabetes ask the same question during consultations:
“Which foods raise my blood sugar quickly, and which ones are safer?”
The glycemic index (GI) is one of the tools used in medical nutrition education to help answer this question. It describes how quickly carbohydrate-containing foods raise blood glucose levels after eating.
When used correctly, glycemic index foods for diabetes blood sugar control can help individuals understand why some meals cause sharp glucose spikes while others lead to more stable readings. However, GI is often misunderstood and sometimes used in a rigid or confusing way.
This page explains the glycemic index clearly, calmly, and practically, focusing on how it can support daily blood sugar management. You’ll also learn why GI works best together with portion size, fiber, protein, and overall meal balance—not replace personalized medical advice.
Why Does Glycemic Index Matter in Diabetes?
The glycemic index is a numerical system that ranks carbohydrate foods based on how fast they raise blood glucose levels compared with pure glucose.
- Glucose is assigned a value of 100
- Foods are then ranked based on how quickly they raise blood glucose after eating
Glycemic Index Categories
- Low GI (55 or less): Causes a slower, more gradual rise in blood sugar
- Medium GI (56–69): Causes a moderate rise
- High GI (70 or higher): Causes a rapid increase in blood glucose
For people with diabetes, low glycemic index foods are generally preferred, as they tend to support more stable post-meal blood sugar levels.
It is important to understand that GI values are measured when foods are eaten alone, under standardized conditions. Real meals are more complex—which is why GI should be used as a guide, not a rule.
Glycemic Index Food Guide for Blood Sugar Control
This table groups common foods by glycemic index (GI) and explains how they
typically affect blood glucose when eaten in usual portions.
Glycemic index values describe how quickly carbohydrate foods raise blood sugar
when eaten alone. Individual blood glucose responses may vary depending on portion
size, meal composition, and personal factors.
Low Glycemic Index Foods (Often suitable for regular inclusion)
| Food Group | Examples | Why They Are Helpful |
|---|---|---|
| Legumes | Lentils, chickpeas, kidney beans | High in fiber and plant protein, which slow digestion and glucose absorption |
| Whole Oats | Steel-cut oats, rolled oats | Contain soluble fiber that helps reduce post-meal blood sugar spikes |
| Fruits | Apples, pears, berries | Natural sugars balanced by fiber for a slower rise in blood glucose |
| Dairy (unsweetened) | Plain yogurt, milk | Protein content slows carbohydrate absorption |
| Whole Grains | Barley, quinoa, whole grains | Less processed and higher in fiber, supporting steadier blood sugar levels |
Clinical note: Low glycemic index foods are often associated with more stable post-meal blood sugar readings and are commonly recommended as part of balanced diabetes-friendly meals.
Medium Glycemic Index Foods (Best eaten with awareness and balance)
| Food | Blood Sugar Consideration | Practical Tip |
|---|---|---|
| Brown rice | Moderate rise in blood glucose | Pair with vegetables and protein |
| Sweet potatoes | Slower than white potatoes but still moderate | Keep portions moderate |
| Bananas | Glycemic index increases with ripeness | Choose less ripe bananas |
| Whole-grain bread | GI varies depending on processing | Combine with eggs, cheese, or healthy fats |
Clinical note: These foods can be part of a healthy diet when eaten in appropriate portions and combined with protein, fiber, or fat to reduce blood sugar spikes.
High Glycemic Index Foods (Require caution, especially when eaten alone)
| Food | Why Blood Sugar Rises Quickly | Safer Use Strategy |
|---|---|---|
| White bread | Highly refined, low fiber | Pair with protein or limit frequent use |
| Instant rice | Rapid digestion | Choose whole-grain alternatives |
| Sugary cereals | Refined carbohydrates and added sugars | Replace with oats or whole-grain options |
| Mashed or fried potatoes | Processing increases glycemic index | Eat with fiber-rich vegetables and protein |
Clinical note: High glycemic index foods are not forbidden, but they are more likely to cause rapid blood sugar increases, particularly when eaten alone or in large portions.
Educational content reviewed by a medical professional. Individual dietary needs should always be discussed with a healthcare provider.
Why Is Glycemic Load Also Important?
One limitation of the glycemic index is that it does not consider portion size. This aspect is where glycemic load (GL) becomes useful.
- GI tells us how quickly blood sugar rises.
- GL tells us how much blood sugar rises based on the amount eaten.
For example, a food may have a high GI but a low glycemic load if consumed in a small portion. In real-world diabetes care, glycemic load often reflects daily eating patterns more accurately than GI alone.
What Affects a Food’s Glycemic Index and How to Use It in Daily Life?
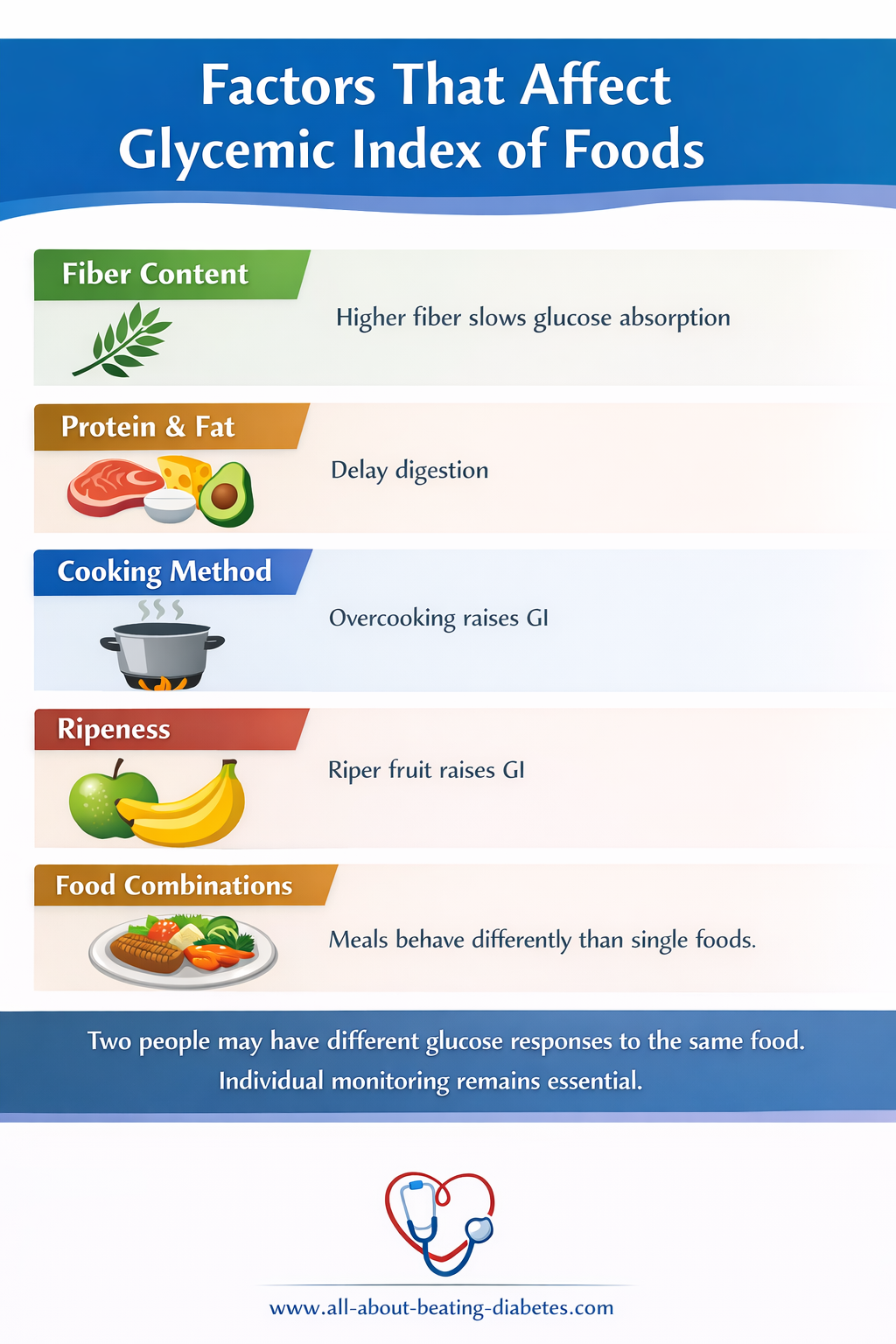
Rather than focusing on numbers alone, a practical medical approach is to:
- Choose low GI foods most of the time
- Combine carbohydrates with protein, fiber, and healthy fats
- Watch portion sizes
- Monitor personal blood glucose responses
- Aim for consistency rather than perfection
Simple Examples:
- Replace white rice with lentils or quinoa
- Pair fruit with yogurt or nuts
- Eat bread with eggs, cheese, or avocado
This approach supports steady blood sugar control without unnecessary restriction.
Common Myths About the Glycemic Index
The glycemic index (GI) is a helpful educational tool, but it is often misunderstood. The table below clarifies some of the most common myths using a practical, medical perspective.
| Common Myth | What You Should Know | Doctor’s Explanation |
|---|---|---|
| “High GI foods are always bad” | Context, portion size, and meal composition matter | High glycemic index foods are not forbidden. When eaten in small portions or combined with protein, fiber, or fat, their effect on blood sugar may be reduced. |
| “GI works the same for everyone” | Individual responses vary | Blood glucose responses differ between individuals due to factors such as insulin sensitivity, gut absorption, activity level, and overall health. |
| “Low GI foods can be eaten freely” | Quantity still matters | Even low glycemic index foods contain carbohydrates. Eating large portions may still raise blood sugar levels, especially in people with diabetes. |
Medical guidance focuses on balance, portion awareness, and personal glucose monitoring rather than strict food rules.
Educational note: Glycemic index is one tool among many. Individual dietary choices should always be guided by blood glucose monitoring and professional medical advice.
Take home notes
- Understanding glycemic index foods for diabetes blood sugar control helps explain why some meals feel easier to manage than others.
- When used alongside portion awareness, balanced nutrition, and regular blood sugar monitoring, the glycemic index can support safer, more confident food choices.
- This content is intended for education and self-management support. Always discuss individual dietary needs with a healthcare professional.
|
Written by Dr.Albana Greca Sejdini, Md, MMedSc Medically reviewed by Dr.Ruden Cakoni, MD, Endocrinologist |
Last reviewed 1/19/2026 |
References
References
- Jenkins DJA, Wolever TMS, Taylor RH, et al. Glycemic index of foods: a physiological basis for carbohydrate exchange. American Journal of Clinical Nutrition. 1981;34(3):362–366.
- Atkinson FS, Foster-Powell K, Brand-Miller JC. International tables of glycemic index and glycemic load values. Diabetes Care. 2008;31(12):2281–2283
- American Diabetes Association. Nutrition therapy for adults with diabetes or prediabetes. Diabetes Care. Updated annually.
- Brand-Miller J, Foster-Powell K, Atkinson F. The New Glucose Revolution. Da Capo Press.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Diabetes diet, eating, and physical activity. U.S. Department of Health & Human Services.
Educational content prepared for general information purposes. Individual glycemic responses may vary. Always consult a healthcare professional for personalized dietary guidance.
Diabetes complications Questions or Problems? Get Help Here
This is the place where you can ask a question about any aspect of diabetes complications.
It's free and it's easy to do. Just fill in the form below, then click on "Submit Your Question".